Progesterone is oestrogen’s partner in managing our important bodily processes. For various social, political and scientific reasons, we have neglected its importance!
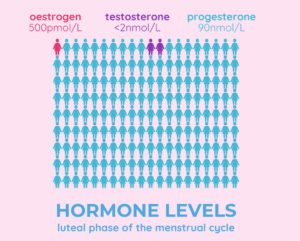
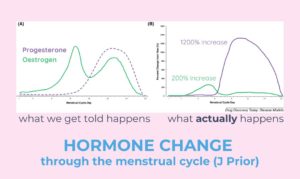
While oestrogen attracts a lot of the spotlight, progesterone is another critical hormone for both females and males. Progesterone levels far exceed those of oestrogen and testosterone and rise by 1-2000% in the luteal phase! Did you know that when you have your blood levels measures, oestrogen and testosterone are reported in “picomols” whilst progesterone is reported in “nanomols” – that is like measuring oestrogen in cents and progesterone in tens of dollars. The graphic below gives an indication of what’s happening during the luteal phase of the cycle (keeping in mind hormone levels fluctuate daily), when progesterone is produced – note how much more progesterone we have than oestrogen and testosterone!
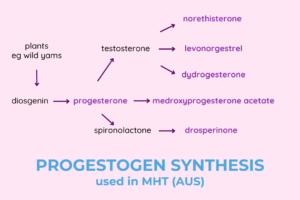
When we refer to “progesterone” we are describing one of the key hormones the body makes during a complex process of steroid hormone production. “Progestogen” describes any compound that will lock into the same progesterone receptor, and includes both “progestins”, which refer to synthetic compounds, and “progesterone” which is formed naturally in the human body. The different progestins have very different properties.
Being synthetic or natural does not mean something is bad or good. Each can be both!
The advantage of progestins is that they are more potent, can be used to control ovulation and can be formulated as a patch or IUD. Body-identical progesterone cannot perform these functions. It cannot be used as contraception, must be micronised to be absorbed and cannot be applied effectively through the skin.
Within the female body, progesterone is predominantly made during the luteal phase of the menstrual cycle within the corpus luteum in the ovary. It is also made in the adrenal glands, the placenta and the brain. Progesterone is mainly metabolised in the liver to various metabolites, most importantly allopregnenolone and pregnenolone. These are active metabolites with important functions.
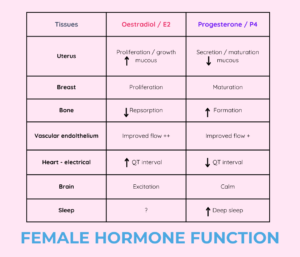
Progesterone is known for its importance in reproduction but at the systemic level, progesterone increases urine production (through activation of the renin-angiotensin system), relaxes smooth muscle cells, raises basal body temperature, has sedative and analgesic effects, improves visual memory, impacts activity of osteoblasts (bone forming cells) and has additionally been found to have a dampening effect on the immune system (anti-inflammatory effect). It counterbalances the proliferative effect that oestrogen has on breast cells and may even be protective against breast cancer.
Reproduction
Progesterone is a key hormone in the reproductive cycle, preparing the endometrial lining for implantation of a fertilised egg. If pregnancy occurs, production of progesterone transfers from the corpus luteum to the placenta itself and remains high right throughout pregnancy. This is an amazingly sophisticated process of positive and negative feedback that we won’t dwell on here.
The brain
Progesterone easily crosses the blood brain barrier and is found in high levels in numerous parts of the brain. There are different types of progesterone receptors, each having varied and complex methods of regulation, each occurring in different areas of the brain. Some are up-regulated by the presence of rising oestradiol such as in the hypothalamus and are involved in the complex feedback mechanism of the menstrual cycle. Some are independent of the oestradiol and the menstrual cycle.
Progesterone and its metabolites (allopregnenolone and pregnenolone) impact brain function via GABA, serotonin and dopamine messaging systems. It is progesterone metabolites made in the liver following oral use that has the benefit if improving sleep. Oestrogen can also interact with these systems.
Effects on mood
Progesterone is often blamed for causing mood disorders, however this is very complex and not fully understood. There are various possible factors including sudden changes in hormone level, absolute levels, different types of progestogens, background sensitivity, tolerance, intercurrent conditions, background mental health conditions and genetics that each play a part. Different women also metabolise progesterone differently to varying quantities of allopregnenolone and pregnenolone.
Around a quarter of women experience premenstrual mood disorders during the late luteal phase where progesterone and oestrogen levels are falling, but typically not when progesterone peaks in the mid luteal phase; premenstrual dysphoric disorder (PMDD) is a severe mood disorder that may extend throughout the luteal phase; some women describe mood disorders on the oral contraceptive pill which may be related to the type of progestogen; during pregnancy, oestrogen and progesterone are high and mood disorders are less common; women with postpartum depression generally have low levels of both oestrogen and progesterone particularly if they are breastfeeding; the postpartum blues which occurs in up to half of all women in the first week after childbirth, are due to sudden progesterone and oestrogen withdrawal.
As you can see the relationship between progestogens and mood is not straightforward.
The cardiovascular system
Progesterone plays an important part in bone and cardiovascular health. Increase QT intervals (a section of the heart rhythm visible on an ECG) is linked to dangerous arrhythmias (“long QT syndrome). Oestrogen causes a lengthening whilst progesterone causes a shortening. Whilst unknown, this may be the mechanism of palpitations noted in perimenopause – a relative increase in oestrogen unbalance by progesterone. Both oestrogen and progesterone improve endothelial function (the way blood flows in vessels).
Bones
Bone is constantly remodelling and we know oestrogen prevents lowering of bone density by reducing the bone resorption side of this process. Progesterone works on the other side by increasing bone formation.
Menopause
When considering the hormonal changes throughout the menopause transition, progesterone is the first sex hormone to fall. In perimenopause, if there is no ovulation, there is no corpus luteum formed and levels of progesterone are very low. This can lead to irregular bleeding, heavy periods, and can be associated with symptoms around the time of the period including hot flushes, exaggerated mood changes, worsening PMS and sleep disorders. This occurs even when oestrogen levels are normal. It is not until the periods spread out and there are more anovulatory cycles that oestrogen levels also start to fall.
Hormonal contraception
Progestogens can inhibit ovulation either on their own as progestin only pills, implants or injections, or in combination with an oestrogen as in the combined hormonal contraceptive pill. Progestogens also modify cervical mucus to prevent pregnancy. Medium dose preparations such as implants and pills maintain oestradiol levels whilst high dose preparations (depot injections) can suppress oestradiol synthesis altogether and can even be associated with reduced bone density.
Menopause hormone therapy
Progestogens are used as part of menopause hormone treatment in two ways.
- To protect the endometrial lining from overstimulation by oestrogen, which may cause hyperplasia and potentially endometrial cancer. If contraception is required, the levonorgestrel IUD or progesterone only pill will also provide contraception.
- Progesterone is a valuable hormone in of itself and has protective impact on bone, the nervous system, and its metabolites can improve mood and sleep in many women.
During perimenopause, progestogens are typically used cyclically for 12-15 days a month, in the luteal phase or second half of the cycle. Bleeding will often (but not always) occur after withdrawal. This DOES NOT inhibit ovulation and your cycle will still be working in the background. It is therefore common to get further irregular bleeding as the hormones in your cycle will change from month to month. For some women in perimenopause, progestogen can be sued daily which is much simpler, accepting some breakthrough bleeding may occur. After menopause, progestogens are used continuously – half the dose given each day.
Micronised progesterone (Prometrium) is now the first choice progestogen as there is a lower risk of breast cancer, clots and mood changes and there is the added benefit for improving sleep. In Australia, it is only available by private prescription. It is effective in protecting the endometrium when used 100mg daily, 200mg for 12-14 days a month and may be used at 300mg daily for treatment of flushes and sleep disturbance. It can be used alone in early perimenopause when the main hormonal change is luteal phase insufficiency (following anovulation) with low progesterone, especially if symptoms are occurring in the last half of the cycle.
What if you think the progestogen in your MHT is causing mood changes?
- Trial a cyclic fashion if you are taking it continuously as this should mean your mood changes are only present when using it and can help confirm your suspicion.
- Switch progestogens – they all have different actions.
- Use a Mirena IUD where only a very small amount is released into the bloodstream
- Switch to tibolone or Duavive (currently not available)
- Switch to an oestradiol / progestin patch (Estalis) as the transdermal route results in different metabolites
- Reduce the oestradiol dose to 12.5mcg which can still protect bones and may treat flushes but needs less frequent progestogen use eg a few times a year
- Use progesterone vaginally which reduces active metabolites (this is an off-label use and requires less frequent dosing as the protective effect occurs locally eg 3 times a week)
- Use non-hormonal therapies
- Having a hysterectomy removes the need for progestin.
Clearly some of these options are quite dramatic! These options are NOT direct medical advice, make sure you discuss any you might consider with your doctor before trialling them to make sure they are safe for you.
References
Physiology, Progesterone. Jessie K. Cable; Michael H. Grider.
This information is for general educational purposes only and does not constitute medical advice. Please see your health professional for advice that is personalised to you.
Key Take Aways
Progesterone is a key female hormone, is present in much greater quantities than oestrogen, but is largely produced in the luteal phase.
“Progestogens” lock into progesterone receptors and include “progesterone” and “progestins”. They can be quite different in their potency and effects.
Progestogens protect the endometrium during MHT and also have specific physiological benefits.
Progestogens can have an impact on mood in some women but the mechanism is unclear.