How safe is it to use MHT after age 65?
The benefits and risks of using long-term menopausal hormone therapy (MHT) lack solid evidence.
Most contemporary guidelines recommend that MHT can be used for as long as the benefits outweighs the risks. This allows for the consideration of personal health issues (such as hormone sensitive cancer or osteoporosis), additional risk factors (such as obesity, family histories) and the presence of ongoing symptoms. These recommendations are largely based on expert consensus informed by current research knowledge, whilst the absolute risks and benefits remain uncertain.
A recent paper explores the health outcomes for women using MHT over the age of 65 years. The study is what we call “observational”. This means that women were not assigned to different intervention groups but reflect the real world – they chose to use MHT for symptom control, their health or on advice of their doctor. The US Centres for Medicare and Medicaid Services database was used and various health outcomes analysed.
For each health outcome, they collected data form one and a half million women still using MHT and nearly a million women not using MHT (controls), so this is a very large study indeed and this strength leads to more reliable results.
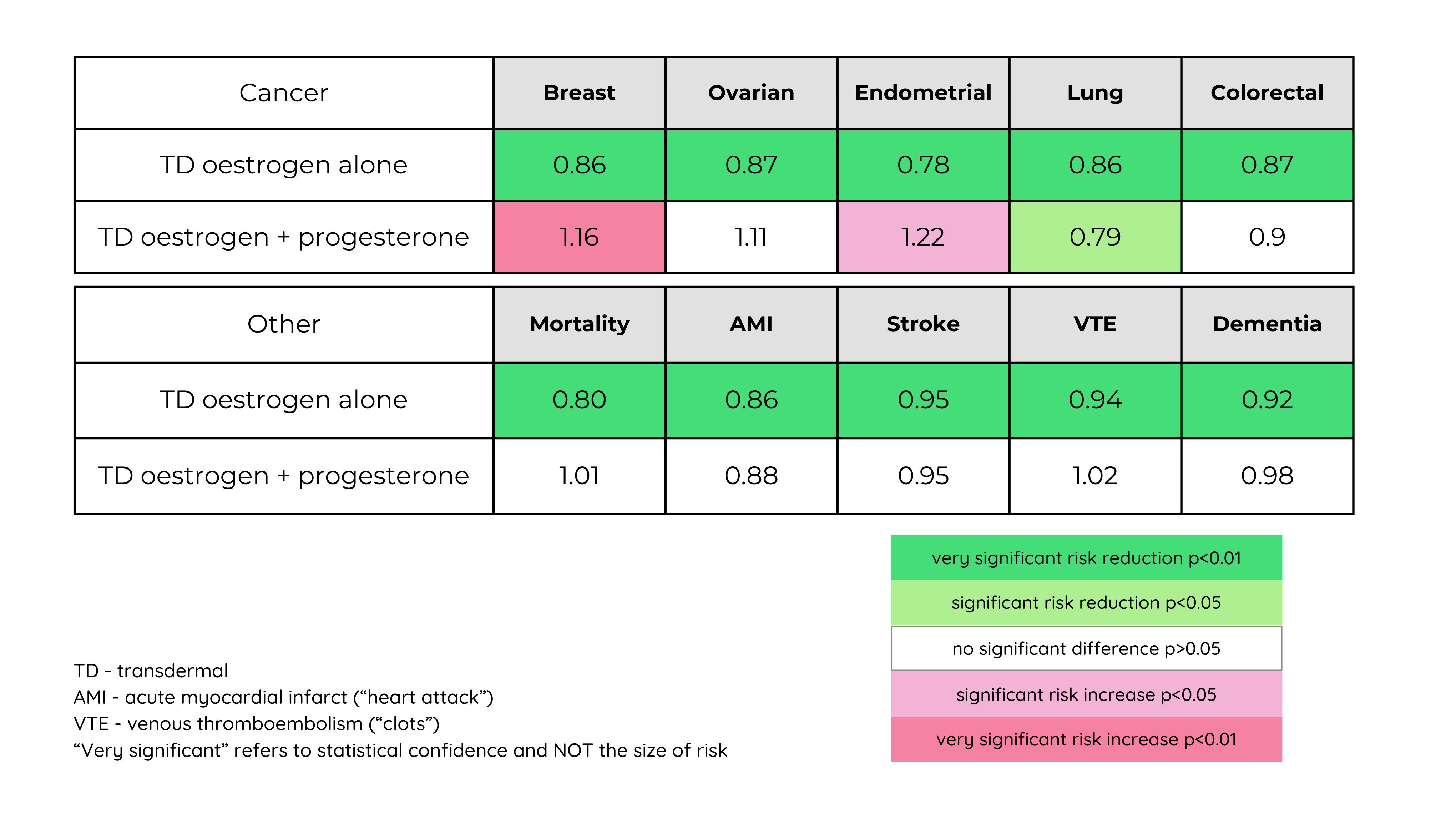
The data allowed type, route and dose of MHT to be analysed. Outcomes included overall mortality, cancer (breast, endometrium, lung, bowel and ovarian), cardiovascular diseases and dementia.
You may be surprised, even confused by some of the results. Remember that scientific knowledge is always evolving, every form of research study has limitations and different populations will show different results. All the information is gathered to inform our best recommendations about benefits and safety. Currently, we could be forgiven for believing that everyone should be using MHT, that it doesn’t increase any cancer risk at all, that it protects your long-term health and that body-identical MHT is safest. We need to keep an open mind to emerging information.
Most women in Australia today use body-identical oestrogen (oestradiol) via transdermal route (patch or gel) in combination with progesterone (a body identical hormone taken as a capsule). This study also explored oral forms of oestradiol, oral conjugated equine oestrogens, vaginal oestrogen and progestins (non-body-identical forms of the natural hormone progesterone). The important results are summarised in the table below which includes selected data from the group using transdermal oestradiol and progesterone.
Women with an intact uterus require protection from developing endometrial cancer by using progesterone or a progestin. Women who have had their uterus removed by hysterectomy, whether they have had their ovaries removed or not, can use oestrogen alone. The use of oestrogen alone and combination menopause hormone therapy appears to have different risks and benefits.
Most women use combination therapy so let’s look at the outcome of this first.
Oestrogen + progesterone MHT
Combination therapy continued after the age of 65 was not associated with an increased risk of mortality, colon cancer, cardiovascular disease or dementia. However, this study does not support combined MHT in reducing the risk of dementia or providing significant heart protection. This study confirms the previously observed increased risk of breast cancer with prolonged use of combination MHT but showed an increased risk with progesterone versus progestin which has not been consistently found in previous research. In contrast to previous observational studies progestin regimes tended to perform better in several other health domains than body identical progesterone.
Interesting observations
Progestins were much more protective than progesterone for endometrial cancer which warrants further research to ensure the safest progesterone regimes for endometrial protection (RR 0.54 decrease v 1.22 increase). This indicates a potential safety concern about progesterone’s adequacy in suppressing the endometrium compared to progestins in MHT. For those at high risk for endometrial cancer, progestins might be preferable.
The use of TD oestrogen plus progestin did not significantly increase the risk of breast cancer however TD oestrogen plus progesterone did.
Oestrogen only MHT
The use of oestrogen alone appears to have multiple benefits including reducing the risk of all cause of death ( mortality), developing cancers ( breast lung and colorectal) many cardiovascular diseases and dementia.
Interesting observations
There was no increased risk of venous thromboembolic disease (VTE) in any users of oestrogen in this study the only increased finding regarding VTE was the use of progestin without oestrogen. Previous data favour trans dermal over oral therapy for a lower clot risk.
Breast cancer risk was most reduced using conjugated equine oestrogen (CEE) at a 23% risk reduction when compared with oestradiol which showed a 12% reduction. This might be explained by the additional oestrogen receptor modulating effects in the various oestrogens contained within CEE.
Links
Read the paper yourself
Use of menopausal hormone therapy beyond age 65 years and its effects on women’s health outcomes by types, routes, and doses.
Baik, Seo H. PhD; Baye, Fitsum MS; McDonald, Clement J. MD. Menopause 31(5):p 363-371, May 2024.
Relative risk of outcomes in women over 65 years by MHT (oestrogen or combination oestrogen + progesterone) compared to non-users.
Limitations
This study was observational in nature and used an extensive database of medical record information however had no data regarding the duration of time using MHT or the status regarding an intact uterus. This means that the data regarding endometrial and even ovarian cancer and the use of various MHT protocols is unreliable. If a woman does not have a uterus, she cannot experience and endometrial cancer, and it would be the hysterectomy and not the use of oestrogen alone that conveyed a benefit.
The use of vaginal oestrogen was associated with the highest risk reductions across all oestrogen types. It is accepted that transvaginal oestrogen is generally not absorbed for systemic effect and therefore any benefit results from some unknown mechanism or more likely, as a result of what is known as “healthy user bias”. This implies that women who are generally healthy, exercise, eat well, seek medical attention and comply with medical recommendations such as using medication, will experience improved overall health. It is unlikely that vaginal oestrogen alone conveys health benefits (risk of urinary tract infections aside).
NOTE
Statistical “significance” is a measure that determines if a result is likely to be a real observation or may have occured simply by chance. Statistical significance is reflected in the P value . Significance does not refer to the size of the effect only the statistical reliability of the observation.
Progestogens are compounds that can lock onto all the body’s progesterone receptors. Progestogens include both progesterone (a body identical hormone) and progestins (synthetical molecules which come from a variety of sources). These have different effects on the cells, much more so than the different types of oestrogens.
Risk. Understanding risk is complicated. Relative risk (RR) ranges from zero upwards. RR of 1.0 indicates that there is no increased or decreased risk. A number between 0 and one indicates there is a decreased risk and a number over one, an increased risk. Relative risk is confusing because when it is expressed as a percentage the magnitude of difference sounds much greater for example a relative risk of two indicates a risk twice as high or 100% greater. A relative risk of 0. 5 indicates half the risk or 50% lower. Relative risk is different to absolute risk. Let’s use the example of breast cancer in women using long term combined MHT. The baseline rate of developing breast cancer is roughly 4 in 1000 women each year, an increase in 20% results in 5 in 1000 women per year, an absolute increased risk of 1 in 1000 women.