THIS INFORMATION IS FOR GENERAL EDUCATIONAL PURPOSES ONLY AND DOES NOT CONSTITUTE MEDICAL ADVICE. PLEASE SEE YOUR HEALTH PROFESSIONAL FOR ADVICE THAT IS PERSONALISED TO YOU.
Key Take Aways
Testosterone can improve distress in HSDD
Its role in improving energy, mood and brain fog is as yet unproven
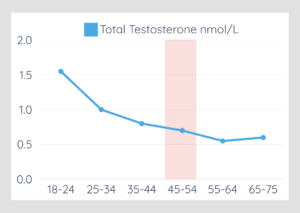
Check blood levels to identify excess and when using testosterone therapy