late perimenopause stage
What’s happening now?
During late perimenopause – you ovulate (release eggs) infrequently (but you can still get pregnant). You have erratic hormone levels with less progesterone and falling levels of oestrogen.
Perimenopause is truly the storm season for hormones but the symptoms won’t last forever.
Perimenopause is the time leading up to your last period and the next 12 months after that. (“Menopause” is actually the day 12 months after your last period, which is a pretty unhelpful definition).
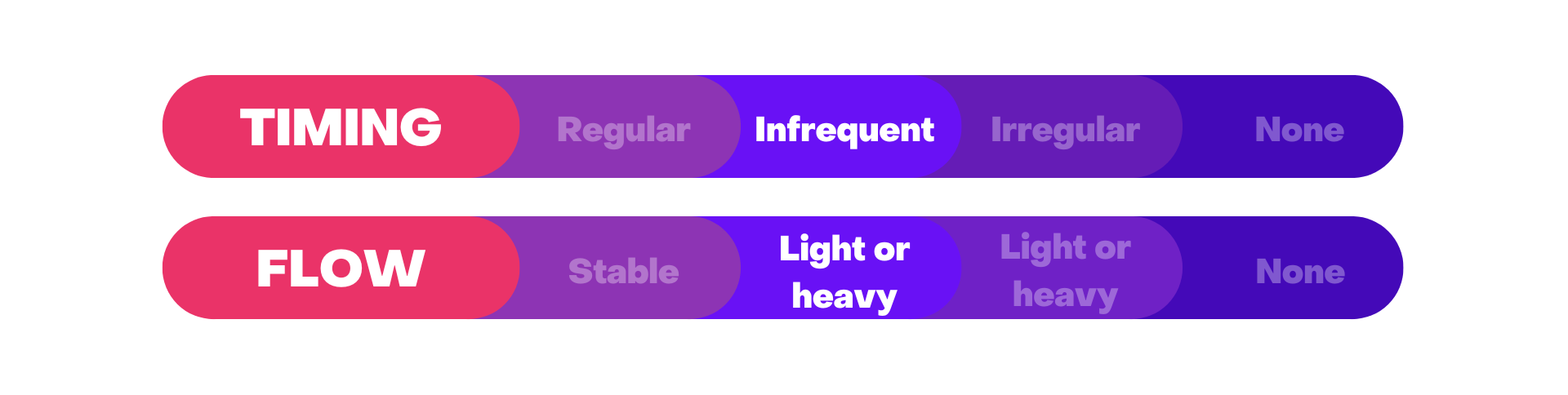
Perimenopause commonly starts in your 40’s. Technically, ‘late perimenopause’ starts when your cycle becomes irregular with more than 60 days between periods.
If you are experiencing spotting between periods, don’t have any symptoms or are under 40, you should check with a doctor whether there may be another cause for the changes in the nature of your period or if you are entering an early menopause.
Mental health problems can also surface now, particularly where there is a background of severe premenstrual mood changes, postnatal depression or a history of clinical depression. It is valuable to consider whether hormone imbalance is contributing, even causing, mood changes as rebalancing hormones can help as a first treatment choice.
The symptoms of early and late perimenopasue are similar. Generally, symptoms of low oestrogen, such as flushes, sweats and vaginal dryness may be more prominent.
These are some of the many symptoms that can arise from falling progesterone and oestrogen
-
Migraines and headaches
-
Disrupted sleep
-
Mood changes
-
Irritability
-
Anxiety
-
Joint and muscle pains
-
Hot flushes, night sweats
-
Breast tenderness
-
Palpitations
-
Weight gain / shift
-
Vaginal dryness
-
Low libido
-
Nerve symptoms like dizziness, odd feelings in your hands and feet
-
Change in body odour
Best treatment for this stage
Now is a perfect time to start getting your lifestyle in order – be active, eat well, get enough sleep, manage your stress.
Many women try over-the-counter supplements but research shows most of these to be only partially effective and some, no better than placebo. If you need more help, hormone treatment can be very effective but this needs to be tailored to your personal symptoms and contraceptive needs. It also needs to be adjusted as you evolve further through the stages.
Healthy habits will make you feel more energetic and brighten your mood in the short term and also protect your health and wellbeing in the years to come. They may also reduce the intensity of menopausal symptoms later.
If you are using the oestrogen containing pill (combined oral contraceptive pill, COCP) for contraception, it can continue to be a great option that not only provides contraception but will control many potential perimenopausal symptoms. This can safely be used in women without contraindications, but should be reassessed if over 50 years, over 35 years and still smoking or if your BMI is over 35.
If you are using the oestrogen containing pill (combined oral contraceptive pill, COCP) for contraception, it can continue to be a great option that not only provides contraception but will control many potential perimenopausal symptoms. This can safely be used in women without contraindications, but should be reassessed if over 50 years, over 35 years and still smoking or if your BMI is over 35.
The COCP is still an option for hormone treatment in women experiencing symptoms of hormone changes during late perimenopause as it overrides brain – ovary communication, provides stable levels of sex hormones, controls heavy or irregular bleeding AND offers contraception at the same time. There are different types of pills depending on your symptoms and if you have been sensitive to pills or other hormonal contraceptives in the past. At some point you will need to switch over to MHT or trial off the COCP with supervision from your doctor.
When your period is coming less frequently, you will almost certainly be having symptoms related to low oestrogen, many of which which may respond to menopause hormone therapy. MHT is often used in a cyclic fashion – progesterone 2 weeks on then 2 weeks off. It will not override your natural cycle – you may still ovulate from time to time. It does not provide contraception.
Women in this stage can often find their period is still heavy and potentially causing some iron loss and fatigue. The progesterone part MHT can be manipulated to control heavy bleeding or you can consider the Mirena IUD , especially of you need contraception. It does make it difficult to assess when your menopause arrives if you are in the majority of women who stop bleeding.
What’s up next?
“Early Menopause” is ahead of you.
Once you have not had a period for 12 months, you are in menopause! Early menopause is the 5 years after your last period.
Symptoms will progressively be due to reduced hormone levels and include more flushes, sweats, vagina and bladder symptoms. Fortunately, many symptoms of hormone imbalance, like mood changes and headaches will start to settle.
A note on blood tests
Unfortunately, blood tests are not very helpful as hormones vary from day to day, week to week, cycle to cycle. Your period, age and symptoms are usually enough to estimate your stage.
If there is doubt as to the cause of your period changes or if you are younger than 45 and are not getting a period, your doctor may order a series of blood tests to explore your cycle and exclude other conditions impacting it.
The hormonal blood tests offer clues but are frequently insufficient to make a clear diagnosis until menopause has been established (there has been no period for 12 months).
This information is for general educational purposes only and does not constitute medical advice. Please see your health professional for advice that is personalised to you.
Key take aways
During the late perimenopause stage each period is coming more than 60 days apart. You may experience some very heavy periods.
Symptoms will start to be due to falling oestrogen as well as progesterone, such as more flushes and sweats.