One of the most distressing issues many menopausal women face is vaginal itching. This can be caused by several conditions, ranging from hormonal changes to infections. Understanding these conditions and their treatments can help you find relief and improve your quality of life.
Normal vaginal flora
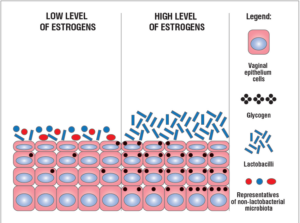
The healthy vaginal microbiome (or flora) has a small, select number of species and is thus very different to the gut microbiome which has a huge number of species.
Before menopause, this healthy balance of bacteria, primarily lactobacilli (which constitutes 95% of vaginal organisms), helps keep the pH level slightly acidic (around 3.8-4.5). This acidity prevents harmful bacteria and yeast from overgrowing. After menopause, declining oestrogen levels lead to a decrease in lactobacilli (specifically inadequate glycogen to feed them) and an overgrowth of other microorganisms, causing the vaginal environment to become less acidic. This change can make women more susceptible to infections like bacterial vaginosis, thrush, and urinary tract infections.
This image demonstrates the changes that result from falling oestrogen.
Evaluation of vaginal microbiota by quantitative real-time PCR. Management of patients with vaginal dysbiosis. Voroshilina, Ekaterina & Plotko, Evgenii & Islamidi, D. & I.V., Lavrenteva & Zornkov, Danila. (2019).
Causes of vaginal itch
1. Genitourinary Syndrome of Menopause (GSM)
Formerly known as vaginal atrophy, GSM is a condition caused by declining oestrogen levels. This hormonal shift leads to thinning and drying of the vaginal walls, which can result in persistent itching, burning, and discomfort.
Treatment:
- Vaginal oestrogen therapy (creams or pessaries).
- Vaginal DHEA pessaries (another hormonal treatment).
- Non-hormonal options like hyaluronic acid.
- Vaginal moisturisers and lubricants for daily relief eg YES or Olive and Bee
- Regular sexual activity or pelvic floor exercises to maintain blood flow to the vaginal tissues.
When using vaginal hormone treatments, they need to be used consistently. GSM is one of the few symptoms of menopause that does not improve over time, typically getting worse.
(You may have heard of vaginal laser – due to the lack of efficacy and safety, all vaginal laser devices have had their TGA approval cancelled).
2. Lichen sclerosis (LS)
LS is a chronic inflammatory skin condition that affects the anogenital region, causing intense itching, white patches, and thinning skin. LS predominantly affects females at a ratio of 5:1 and is associated with autoimmune diseases such as autoimmune thyroid disease, vitiligo, and psoriasis. If left untreated, it can lead to scarring and discomfort during intercourse.
Treatment:
- Prescription corticosteroid creams applied twice weekly to reduce inflammation.
- Regular monitoring by a healthcare provider, as there is a small risk of vulvar cancer.
- Emollients to keep the area moisturised.
3. Vaginal thrush (yeast infection)
Candida overgrowth can lead to vaginal thrush, a common cause of intense itching, burning, and sometimes a thick, white discharge. Menopausal hormone therapy or vaginal oestrogen may increase the risk of thrush as it results in increased vaginal cellular glycogen production, a fuel for candida growth. Using antibiotics can also interfere with the normal flora and result in thrush for some women.
Treatment:
- Over-the-counter antifungal creams or pessaries (e.g., miconazole, clotrimazole).
- Prescription oral antifungals like fluconazole for recurrent infections.
- Avoiding irritants such as scented soaps and wearing breathable cotton underwear.
4. Bacterial vaginosis (BV)
BV occurs when there’s an imbalance in the vaginal bacteria, leading to itching, irritation, and a fishy-smelling discharge (although more than 50% of women have no symptoms). Whilst it is not a sexually transmitted disease, sexual activity increase your risk and recent research suggests treating male sexual partner may also be helpful in preventing recurrence.
Treatment:
- Prescription antibiotics like metronidazole or clindamycin.
- Avoiding douching and strong detergents that disrupt vaginal bacteria.
- Treating male sexual partners may reduce the risk of recurrence.
Gardnerella vaginalis, Mobiluncus species and Prevotella species are the most typical causes of BV.
5. Contact dermatitis & allergies
Skin reactions to soaps, detergents, scented toilet paper, or even certain fabrics can cause vaginal itching.
Treatment:
- Identifying and eliminating the irritant.
- Using hypoallergenic and fragrance-free products.
- Applying a soothing barrier cream like petroleum jelly or zinc oxide.
When to see a doctor
While mild irritation can often be managed at home, seek medical advice if itching is severe or persistent; you notice abnormal discharge, bleeding, or skin changes; or symptoms don’t improve.
A word on vaginal probiotics
The use or benefit of vaginal probiotics remain controversial. Probiotics taken orally have not been shown to impact the vaginal flora and research into vaginal application shows mixed results.
Vaginal itching during menopause is common but manageable. Identifying the underlying cause is the first step toward effective treatment. Whether it’s due to GSM, lichen sclerosus, infections, or irritants, there are solutions available to help you feel comfortable again. If you’re experiencing persistent symptoms, don’t hesitate to reach out to a healthcare provider for guidance.